Understanding Type 1 Diabetes
Type 1 diabetes, also known as insulin-dependent diabetes, is a chronic autoimmune disease where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the body is unable to produce sufficient insulin, leading to elevated blood sugar levels since insulin is essential for regulating glucose. While type 1 diabetes is frequently diagnosed in children and young adults, it can develop at any age. Unlike type 2 diabetes, which stems from insulin resistance and is often linked to obesity and physical inactivity, type 1 is driven by autoimmune factors.
Causes and Risk Factors

The exact cause of type 1 diabetes remains unclear, but it is believed to be influenced by a combination of genetic and environmental factors. Common risk factors include a family history of the disease, genetic predisposition, and possible exposure to certain viruses. Other potential contributors may include high blood pressure, obesity, and diets high in sugar and refined carbohydrates. Ongoing research aims to further identify additional risk factors and to develop new treatments for better management of the disease.
Symptoms and Diagnosis

Symptoms of type 1 diabetes often develop suddenly and can include increased thirst, frequent urination, fatigue, and blurred vision. If left untreated, type 1 diabetes can result in severe complications like diabetic ketoacidosis and kidney damage. Diagnosis typically involves a physical exam, a review of medical history, and blood tests to measure blood glucose levels. The presence of autoantibodies against insulin and other pancreatic proteins is often used to confirm the diagnosis, indicating the autoimmune nature of the disease.
Managing Blood Glucose Levels

Managing blood glucose levels is a crucial aspect of diabetes management for people with type 1 diabetes, as prolonged high blood sugar can cause serious complications. This is typically managed through a combination of insulin injections, a healthy diet, and regular physical activity. Utilizing continuous glucose monitoring (CGM) allows for tracking blood sugar levels throughout the day, helping to identify trends and patterns. By adjusting insulin doses and meal plans based on CGM data, individuals can achieve better blood glucose control and reduce the risk of complications.
Complications and Long-term Effects
Unmanaged type 1 diabetes can result in serious complications such as nerve damage, kidney damage, and eye damage. Persistently high blood sugar levels also increase the risk of heart disease, stroke, and other cardiovascular conditions. Regular check-ups with a healthcare provider are essential to detect and prevent complications early. Maintaining good blood glucose control helps reduce the risk of these complications and supports overall health.
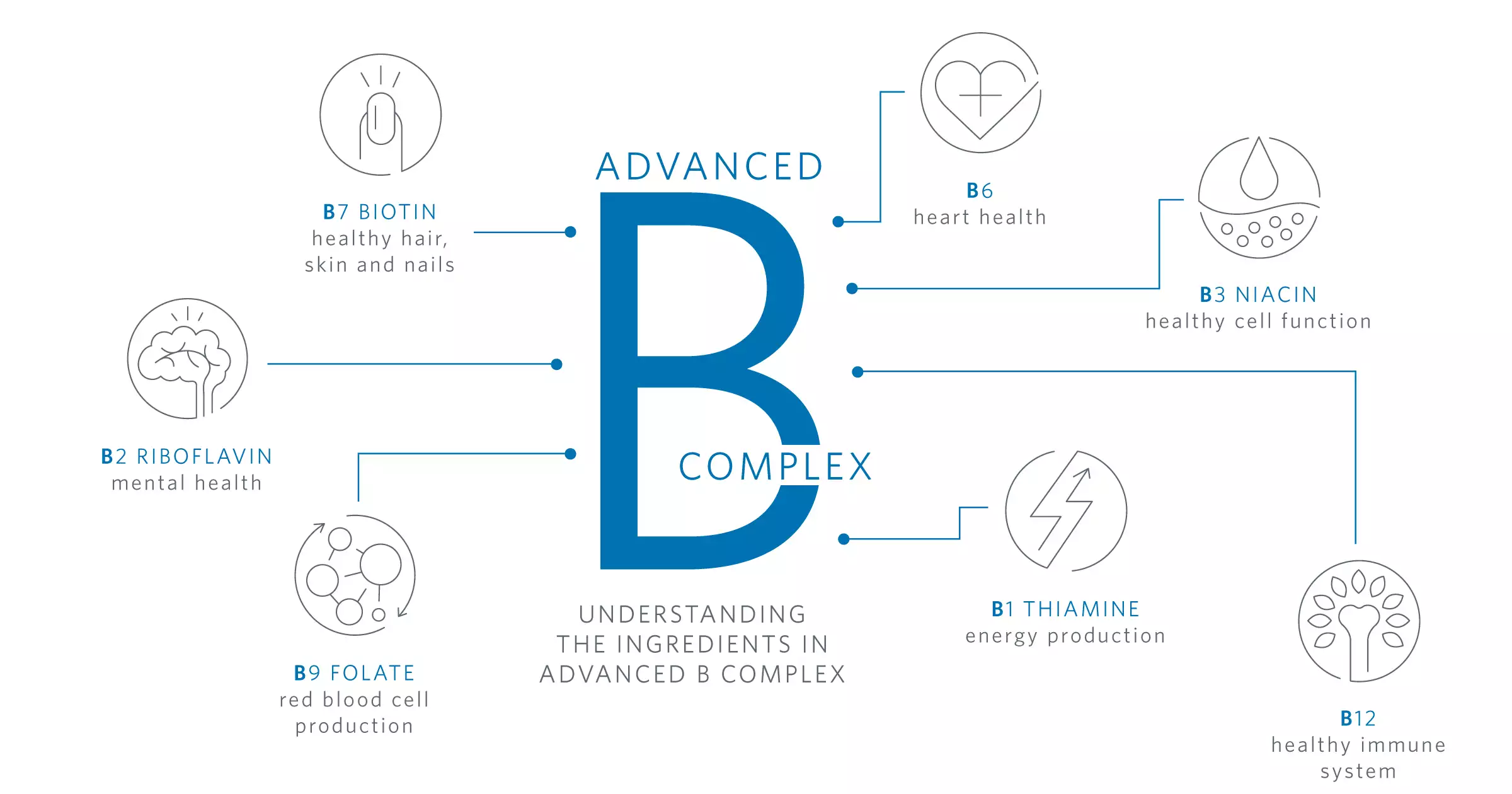
Treatment and Management Options

Insulin therapy is the primary treatment for type 1 diabetes, requiring insulin injections to regulate blood glucose. Types of insulin include rapid-acting, short-acting, and long-acting. Additional management tools like insulin pumps and continuous glucose monitoring (CGM) systems can improve control. Other treatments, such as oral medications, inhaled insulin, and immunotherapy, are also being explored.
Lifestyle Changes and Self-Management

Healthy lifestyle changes are vital for managing type 1 diabetes. Low blood sugar, or hypoglycemia, can occur as a side effect of insulin treatment, making it important to recognize and manage its symptoms effectively. This includes following a healthy diet, engaging in regular physical activity, and maintaining a healthy weight. Stress management techniques like yoga and meditation can also help stabilize blood glucose. Self-management skills, such as tracking blood glucose levels and adjusting insulin doses, are crucial for effective diabetes care.
Finding the Right Doctor and Care Team

A strong care team is essential for managing type 1 diabetes. This team may include an endocrinologist, a registered dietitian, and a certified diabetes educator. They provide personalized treatment plans, ongoing support, and guidance on self-management. Emotional support and assistance with day-to-day care are also part of the care team’s role.
Advances in Research and Treatment

Research is continuously advancing to develop new treatments for type 1 diabetes, including immunotherapy and stem cell therapy. Technological advances like CGM systems and insulin pumps are improving blood glucose control. Ongoing clinical trials are testing new therapies, with organizations like the American Diabetes Association working to raise awareness and promote education.
Prevention and Outlook

Although there is no known way to prevent type 1 diabetes, maintaining good blood glucose control can reduce the risk of complications. Research advancements are improving the outlook for people with type 1 diabetes, enabling them to lead long, healthy lives with proper management and care.
Conclusion
Type 1 diabetes is a chronic autoimmune disease that requires continuous management. While prevention remains elusive, ongoing research is leading to promising new treatments. By making healthy lifestyle changes, managing blood glucose levels, and collaborating with a healthcare provider, individuals with type 1 diabetes can reduce complications and improve their quality of life.